More than 36,000 Te Whatu Ora nurses, midwives, health care assistants and kaimahi hauora have voted to strike for 24-hours after Health NZ failed to address their safe staffing concerns.
New Zealand Nurses Organisation Tōpūtanga Tapuhi Kaitiaki o Aotearoa (NZNO) Chief Executive Paul Goulter says there was strong support from members to take strike action after a new offer from Te Whatu Ora last week was worse than a previous one in May.
"This latest offer from Te Whatu Ora fails to address concerns about safe staffing despite them being raised continually throughout the collective agreement bargaining process.
"Patients are at risk because of short staffing. Nurses, midwives and health care assistants are stretched too thin and can’t give patients the care they need. This is heartbreaking for our exhausted members who became health care workers because they want to help people.
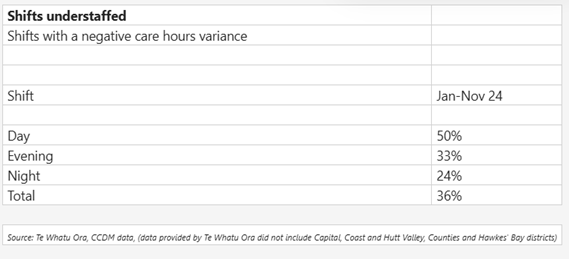
"Te Whatu Ora data obtained by NZNO under the Official Information Act shows between January and November last year, 50% of all days shifts were understaffed across hospital wards in 16 health districts," Paul Goulter says. (see table in editor’s notes)
To "add insult to injury" members have again been offered a wage increase which doesn’t meet cost of living increases and will see them and their whānau go backwards financially, he says.
"There were 30,000 New Zealanders who moved to Australia in the past year. We know some of them are burnt out nurses moving for better conditions and wages.
"Te Whatu Ora needs to do more to retain our nursing workforce, employ graduate nurses and ensure patients get the care they need. This is about the health and wellbeing of real people and their whānau, not the need to meet some arbitrary budget set by the Government.
"It looks like this Government has lost control of health," Paul Goulter says.
Editor notes:
-The nationwide strike will be held from 9am on Wednesday 30 July until 9am on Thursday 31 July.
-The strike will be a complete withdrawal of labour at every place in New Zealand where Te Whatu Ora provides health care or hospital care services.
-Life preserving services will continue to be provided.